Clinical Quality Measures CQM: Framework for Healthcare Performance Reporting
Clinical Quality Measures CQM serve as the foundation of healthcare performance reporting, allowing providers to quantify patient outcomes, enhance care delivery, and meet regulatory requirements. These standardized measures encompass eCQMs and HEDIS to MSSP ACO and ACO REACH programs, and they assist organizations to attain improved patient outcomes and remain compliant with various quality reporting programs.
Healthcare providers are under increasing pressure to show quantifiable changes in patient care and operate within complicated regulatory environments. Clinical Quality Measures CQM are the standardized model that converts raw patient data into actionable information, allowing healthcare organizations to monitor performance, detect care gaps, and fulfill strict reporting criteria in various programs.
The current healthcare quality reporting requires accuracy, real-time tracking, and the ability to integrate different platforms and programs. These measures are the basis of value-based care initiatives, starting with eCQMs that capture electronic health record data and ending with full-scale HEDIS reporting to managed care organizations. Organizations that are members of the MSSP ACO and ACO REACH programs use these standardized measures to show their dedication to better patient outcomes and cost control.
What Are Clinical Quality Measures (CQM)?
Clinical Quality Measures are standardized performance measures that evaluate the quality of healthcare services provided to patients. These measures assess certain areas of care such as clinical processes, patient outcomes, patient safety, and care coordination.
Quality measures fall into several distinct categories:
- Process measures: Track whether healthcare providers follow established best practices
- Outcome measures: Evaluate the results of healthcare interventions
- Structure measures: Assess healthcare system capabilities and resources
- Patient experience measures: Capture patient perspectives on care quality
The Centers of Medicare and Medicaid Services (CMS) mandate healthcare providers to report on certain quality measures to be eligible to join federal programs and be paid on a performance basis.
Types of Quality Reporting Programs
Healthcare organizations have to deal with various reporting requirements in various programs, and eCQMs are the basis of electronic reporting, where data is collected directly in electronic health records to simplify the measurement process.
- HEDIS measures focus on managed care performance across six domains of care, including effectiveness of care, access to care, and patient experience. Health plans use these measures to demonstrate value to employers and consumers.
- MSSP ACO participants track 33 quality measures across four domains: patient safety, care coordination, preventive health, and at-risk populations. Organizations must meet quality thresholds to share in Medicare savings.
- ACO REACH programs emphasize health equity and advanced primary care, requiring participants to report on both traditional quality measures and social determinants of health indicators.
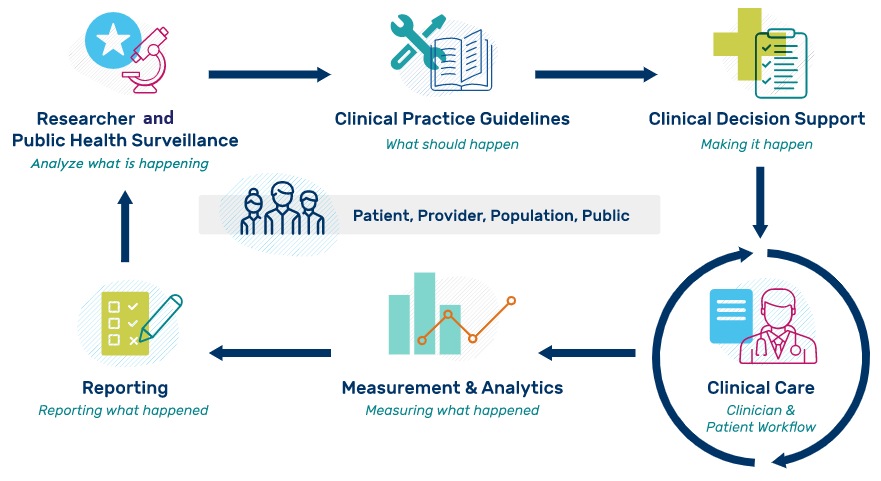
How CQM Works?
The calculation of quality measures is a systematic process that converts patient data into meaningful performance measures. It starts with the collection of data through various sources, such as electronic health records, claims data, and patient registries.
Normalization of data provides uniformity between systems and formats. This step standardizes terminology, fixes errors, and aligns patient records across various data sources to form complete patient profiles.
The Measurement Process
Healthcare organizations implement a structured approach to quality measurement:
- Data acquisition captures structured and unstructured information from all relevant sources
- Patient identification determines which patients qualify for specific measures
- Numerator calculation counts patients who received recommended care or achieved target outcomes
- The denominator calculation identifies the total eligible patient population
- Performance rate calculation divides the numerator by the denominator to determine compliance rates
Advanced systems employ artificial intelligence and natural language processing to extract relevant information from clinical notes, improving measurement accuracy and reducing manual abstraction requirements.
Benefits of Implementing Clinical Quality Measures
There are several benefits that healthcare organizations gain by adopting extensive quality measurement programs. The systematic identification of care gaps and evidence-based interventions leads to patient care improvements.
Monetary rewards are performance-based incentive payments, shared savings opportunities, and lessening penalties on non-compliance. Companies that are good at quality reporting tend to get better reimbursement rates and bonuses.
Operational Improvements
Quality measurement drives operational efficiency through:
- Care standardization across providers and locations
- Resource allocation based on patient needs and risk profiles
- Provider performance monitoring and improvement initiatives
- Patient engagement through transparent quality reporting
Proactive intervention before quality metrics deteriorate can be supported by real-time monitoring capabilities, which can be used to support continuous improvement initiatives.
Regulatory Compliance
Comprehensive quality measurement ensures compliance with federal requirements while positioning organizations for success in value-based care contracts. Organizations avoid penalties while qualifying for performance bonuses and shared savings opportunities.
Key Quality Measure Categories
Quality measures are categorized into particular groups that emphasize various areas of healthcare performance. All categories make sure that providers are oriented to the enhancement of clinical outcomes and patient experiences and remain in line with regulatory requirements.
Promoting Interoperability
It measures how effectively healthcare providers use certified electronic health record technology to improve patient care. These measures focus on electronic prescribing, health information exchange, and patient access to health information.
Healthcare providers must demonstrate meaningful use of EHR systems through specific performance thresholds. PI reporting directly impacts Medicare reimbursement rates and quality scores.
HEDIS Quality Measures
HEDIS measures evaluate health plan performance across multiple domains of care. These standardized measures enable comparison between health plans and track industry-wide performance trends.
Key HEDIS measure categories include:
- Effectiveness of care: Clinical quality and appropriateness of services
- Access and availability: Timely access to care and provider availability
- Experience of care: Patient satisfaction and engagement metrics
- Utilization patterns: Healthcare service usage and efficiency
- Health plan descriptive information: Membership and provider characteristics
ACO Performance Measures
MSSP ACO and ACO REACH programs emphasize population health management and care coordination. These programs need to be reported in a comprehensive manner in various quality areas and be cost-effective.
The participants of ACO REACH are required to show the improvement of health equity measures, which are social determinants of health that influence patient outcomes. These programs are the development of further value-based care models.
Implementation Strategies
Quality measures cannot be implemented only with technology, but they need a systematic approach that incorporates data, workflows, and reporting tools. Powerful strategies assist healthcare organizations in attaining precision, adherence, and sustained enhancement in performance results.
Data Integration and Management
Effective quality measure implementation needs strong data integration. Healthcare organizations need to integrate electronic health records, claims systems, patient registries, and external data sources into integrated platforms.
Patient identity matching across multiple systems ensures accurate measure calculation and prevents duplicate counting. High-level enterprise master patient index (eMPI) systems eliminate patient identity conflicts and ensure data integrity.
The data cleansing procedures detect and rectify errors, inconsistencies, and missing data that may affect the accuracy of measurements. Automated validation rules indicate possible data quality problems to be reviewed and corrected.
Technology Infrastructure
The current digital health systems offer full quality measure management features, combining data collection, measure computation, care gap detection, and reporting features into a single system.
These platforms utilize advanced algorithms to handle vast amounts of healthcare data without compromising accuracy or adherence to industry standards. Real-time processing features enable real-time feedback to providers and care teams.
Workflow Integration
The success of quality measures relies on the smooth integration with clinical workflows. During patient encounters, healthcare providers must have access to patient-specific quality measures and care gap data in real-time.
The automated generation of tasks and care team notifications will provide timely follow-up on quality measure opportunities. Clinical decision support systems integration offers evidence-based recommendations at the point of care.
Reporting and Analytics
Raw data must be transformed into actionable insights through accurate reporting and powerful analytics. These tools provide organizations with the transparency to gauge progress, performance, and make informed decisions to improve quality in the long term.
Performance Dashboards
Healthcare organizations need to have a full picture of quality measure performance in various dimensions. Executive dashboards give top-level organizational performance indicators, whereas departmental views concentrate on the appropriate measures and areas of improvement.
Provider-level reporting allows monitoring of individual performance and specific improvement efforts. Patient-level analytics facilitate care gap closure and population health management strategies.
Benchmarking and Comparisons
Quality measure reporting involves comparison with national standards, regional averages, and peer organizations. Such comparisons assist healthcare leaders in knowing how they perform in comparison to others and where they can improve.
Trend analysis reveals performance patterns over time, supporting strategic planning and resource allocation decisions. Statistical process control methods identify significant performance changes requiring immediate attention.
Challenges and Solutions
Data Quality Issues
Healthcare organizations frequently encounter data quality challenges that impact measurement accuracy. Missing documentation, coding errors, and incomplete patient records can significantly affect performance scores.
Natural language processing technologies extract relevant information from unstructured clinical notes, improving measure capture rates and reducing manual abstraction requirements. Advanced algorithms identify potential documentation gaps and prompt providers to complete required information.
Resource Requirements
Quality measure implementation requires significant investment in technology infrastructure, staff training, and ongoing maintenance. Organizations must balance resource allocation between quality improvement initiatives and operational requirements.
Integrated platforms reduce resource requirements by combining multiple quality reporting functions into unified systems. Automated processes minimize manual intervention while maintaining accuracy and compliance standards.
Regulatory Changes
Specifications of quality measures are dynamic, and organizations have to revise systems, processes, and training materials. Keeping up with regulatory demands requires specific resources and skills.
The advantages of collaborating with specialized vendors are that they are up to date with the regulatory requirements and offer timely updates to the system. This method minimizes the internal resource needs and provides compliance.
Measuring Success
In order to achieve the best results of Clinical Quality Measures, organizations should monitor the progress using clear benchmarks. The definition of success is based not only on compliance but also on the regular improvement of patient outcomes, provider engagement, and financial performance.
Key Performance Indicators
Healthcare organizations track multiple metrics to evaluate quality measure program success:
- Measure compliance rates across all reporting requirements
- Care gap closure percentages for targeted interventions
- Provider engagement levels with quality improvement initiatives
- Patient outcome improvements linked to quality measure performance
- Financial performance, including incentive payments and shared savings
Frequent performance review meetings will hold accountability and will promote continuous improvement among all stakeholders.
Continuous Improvement
Quality measure programs need continuous improvement and optimization. Organizations examine performance trends, find areas of improvement, and apply specific interventions to improve performance.
The most successful organizations have quality committees that review, measure performance, analyze root causes of quality gaps, and create evidence-based improvement strategies. These committees consist of clinical leaders, quality professionals, and operational staff.
Bottom Line
Clinical Quality Measures (CQM) are the cornerstone of contemporary healthcare performance reporting, allowing organizations to show value and enhance patient outcomes in various regulatory programs, such as eCQMs, HEDIS, MSSP ACO, and ACO REACH programs.
Persivia delivers the comprehensive solution healthcare organizations need to excel. Our unified platform integrates advanced algorithms, powerful normalization, and real-time monitoring to assist you in measuring, enhancing, and reporting on quality measures with greater precision than ever before. Having demonstrated outcomes of 91% exceptional MIPS scores versus the 82% national average, Persivia is turning quality reporting into a competitive edge rather than a compliance liability.